Call us: +86-137-2353-4866
New sensor technology helps blood pressure monitors work better and feel nicer. People now use small, wearable devices instead of big cuffs. These new devices fit into daily life easily. Healthcare workers like real-time data. It helps them find health problems early and act fast. Recent studies show these new devices are as accurate as old ones.
| Device | Technology | Study Year | Accuracy and Validation Results |
|---|---|---|---|
| Aktiia Bracelet | PPG smartwatch | 2021 | Met ISO81060-2 validation criteria in sitting position. |
| CareUp® | Photoplethysmography (PPG) | 2019 | Accuracy similar to oscillometric devices. |
SOUSHINE is leading this change. They use force sensing and force sensing sesistor technology. Their new ideas make health tracking easier and more trustworthy.
Key Takeaways
- New sensor technologies like MEMS and multi-element sensors help check blood pressure all the time. They do not need big cuffs. They are accurate and comfortable.
- Continuous monitoring gives real-time data. This helps doctors find hidden hypertension. Doctors can change treatments fast to stop heart problems.
- Hybrid sensor systems use tonometry, optical, and magnetic sensors with AI. This makes blood pressure checks more correct during daily activities.
- Flexible, wearable devices use soft materials. People can check blood pressure all day. They can do this even when sleeping or exercising. These devices do not hurt.
- Mobile apps connect to wearables. They show easy charts. Doctors can watch patients from far away. This helps patients get care faster.
- Clinical studies show wearable devices can check blood pressure well. But they still need more testing and approval from regulators.
- Continuous monitoring helps patients by giving real-time feedback. This helps people control hypertension and make better habits.
- In the future, new materials and AI will make wearable blood pressure monitors better. They will be more sensitive, last longer, and fit each person for better health tracking.
Why Continuous Monitoring Matters
Real-Time Health Insights
Real-time monitoring lets people and doctors see blood pressure changes all day. It shows how blood pressure goes up or down during things like exercise, stress, and sleep. Doctors can spot patterns and what causes hypertension. They can change treatment fast if needed. Real-time monitoring checks if medicine and healthy habits are working. Remote patient monitoring uses this data to plan care and find problems early. These programs also help patients learn how their actions affect their health. People see how stress, food, and exercise change their blood pressure. This helps them make better choices and lowers the chance of heart problems.
- Real-time monitoring finds blood pressure changes that single checks miss.
- Doctors use this information to stop serious heart problems.
- Patients feel more in control and can act faster.
Real-time monitoring helps people stop problems before they start. This way, health gets better and patients are happier.
Hypertension Risks
Hypertension affects about 1.39 billion adults around the world. Many people do not know they have it because there are no signs. This condition raises the risk of heart disease, stroke, and kidney issues. The risk is higher where people cannot get good health care or healthy food. Checking blood pressure often helps find hypertension early. Finding it early means better control and fewer health problems. Studies show that continuous monitoring predicts heart problems better than office checks. Checking at night and all day gives the best information about risk. Doctors use this data to pick the best treatment and stop problems.
- Hypertension is a top cause of heart disease.
- Continuous monitoring helps doctors find hidden hypertension and treat it better.
- Acting early can save lives and lower health care costs.
Traditional Limitations
Traditional cuff monitors only check blood pressure at certain times. They cannot track changes during daily life or sleep. Many people think cuffs are not comfortable. If the cuff does not fit right, it can be wrong. Some people do not use them the right way, so mistakes happen. These monitors cannot check blood pressure during exercise, driving, or stress. Because of these limits, important changes may not be seen. Continuous monitoring fixes these problems. It gives a full view of blood pressure and helps manage hypertension better. Better monitoring means better health and fewer heart problems.
- Traditional monitors miss important blood pressure changes.
- Continuous monitoring is more accurate and comfortable.
- People get better care and have a lower risk of heart problems.
Sensor Breakthroughs
MEMS and Tonometry
MEMS are very small machines that help check blood pressure in new ways. Tonometry checks blood pressure by pressing a sensor on the skin over an artery. This way does not need a cuff. It gives real-time data and works well for non-invasive checks.
New MEMS and tonometry have changed how people watch their blood pressure. Companies made wearable MEMS 3-axis force sensor arrays. These sensors use a triaxial adjustment system. They block noise from body movement and give steady readings. The standard deviation stays low, even when people move.
SOUSHINE’s high-precision multi-element MEMS pressure sensor uses 46 sensing elements. Each element works with an ASIC that has multiplexers, operational amplifiers, and filters. This design uses fewer electrodes. It also blocks noise better and makes the device smaller. New packaging keeps the sensor safe from stress and keeps it accurate. These changes let people check blood pressure all the time using tonometry. Now, people can use these sensors in wrist-wearable devices, not just in clinics.
MEMS and tonometry together make blood pressure checks easier, more comfortable, and more accurate.
Multi-Element Sensors
Multi-element sensors have many sensing parts, not just one. This design helps measure blood pressure better. For example, a three-axis tactile force sensor can sense forces in three ways: x, y, and z. This means the sensor can measure the total force on the artery, no matter how it sits.
Single-element sensors only measure force in one way. They need careful placement and can give different results if moved. Multi-element sensors do not have this problem. They give the same results even if the angle or position changes. This makes calibration easier and improves reliability.
Studies show that multi-element sensors match the accuracy of cuff-based devices. The readings stay within 5 mmHg of standard devices. The sensors also help with continuous, non-invasive blood pressure monitoring. They let users check their blood pressure at any time, even during sleep or exercise. This level of accuracy and reliability supports better health management.
Flexible and Wearable Designs
Flexible and wearable sensor designs help people check blood pressure all day. These sensors use soft materials like PDMS that bend and move with the skin. The sensors stay comfortable and do not cause irritation.
A recent study tested a flexible capacitive pressure sensor made with PDMS and deionized water. The sensor had high sensitivity and a fast response time. It worked well for over 50 minutes at different pressures. The study included 160 people of different ages, heights, and weights. The sensor captured blood pressure waveforms across a wide range of values. It met all international standards for accuracy when compared to standard devices.
| Evidence Aspect | Details |
|---|---|
| Sensor Composition | Capacitive pressure sensor using PDMS and deionized water (DIW), enhanced with baking powder |
| Sensitivity | 0.021 Pa⁻¹ |
| Detection Limit | 1 Pa |
| Response Time | 100 ms |
| Operational Stability | Stable over 50 minutes at multiple pressures (100 Pa to 30 kPa) |
| Clinical Validation Participants | 160 individuals with diverse ages, heights, and weights |
| Clinical Validation Outcomes | Successfully captured oscillometric waveforms (OMW) across wide BP ranges |
| Accuracy Compared to Standards | Met all criteria of AAMI/ESH/ISO universal standard when compared with OMRON and mercury sphygmomanometer |
| Pulse Rate Measurement | Accurate and consistent with reference devices |
| Sensor Flexibility and Wearability | High flexibility due to porous PDMS dielectric layer, suitable for skin contact and wearable applications |
| Additional Features | Porosity introduced in PDMS layer improves flexibility and sensor performance |
Flexible sensors make non-invasive blood pressure checks possible every day. People can wear these sensors on their wrists or arms. The sensors keep working during movement, sleep, or exercise. This design supports continuous, high-precision monitoring and helps users manage their health better.
Hybrid Sensor Systems
Hybrid sensor systems are changing how people check blood pressure. These systems mix different sensors and smart data tools. They use tonometry, optical sensors, magnetic sensors, and AI models. Each part helps the system work better.
Tonometry is very important in hybrid sensor systems. It checks pressure by pressing a sensor on the skin over an artery. This way gives direct blood pressure readings. When engineers add other sensors to tonometry, they get more data. Optical sensors like PPG watch blood flow and pulse rate. Magnetic sensors pick up strong signals and do not get mixed up by light. Using tonometry with these sensors makes the information more correct.
Hybrid systems also use deep learning models. These models include convolutional neural networks and BiLSTM. They look at signals from tonometry and other sensors. The models find patterns in the signals. They help the system guess blood pressure very well. Some systems have mean errors as low as 1.69 mmHg for systolic pressure. This good accuracy helps with non-invasive, all-day monitoring.
Engineers often use tonometry with ECG and PPG signals. They find features like Pulse Transit Time. This feature is closely linked to blood pressure. But signals can change if people move or have different skin. Deep learning helps fix these problems. It learns from lots of examples and changes with new data. This makes hybrid systems work better.
The table below shows how each part helps the system:
| Technology Component | Contribution to Hybrid Sensor System | Benefit for Blood Pressure Monitoring |
|---|---|---|
| Tonometry | Direct pressure measurement at the artery | Real-time, beat-by-beat blood pressure data |
| Magnetic Sensors | Strong signal capture, resist light interference | Better signal quality and reliability |
| Optical Sensors (PPG) | Track blood volume and pulse rate | Extra physiological data for blood pressure estimation |
| Multi-sensor Data Fusion | Combine signals from tonometry and other sensors | Improved accuracy and data interpretation |
| AI-driven Models | Analyze hybrid signals, learn complex patterns | Higher accuracy and robustness |
| Wearable Device Design | Compact, skin-friendly integration of tonometry and sensors | Easy, comfortable, and continuous monitoring |
Hybrid sensor systems use tonometry in many ways. Some systems use a soft patch that sticks to the skin. This patch collects tonometry, ECG, and PPG signals at once. The patch sends all the data to a small computer. The computer uses deep learning to guess blood pressure. This setup works well for daily life.
Tonometry helps hybrid systems work in real situations. It gives direct pressure readings, even when people move or sleep. When used with other sensors, tonometry fills in missing data. This teamwork helps track blood pressure better.
Hybrid systems also help with mobile health. People can wear these devices all day. The system sends data to a phone or cloud. Doctors and users see blood pressure changes right away. Tonometry keeps the data correct, even during daily activities.
Hybrid sensor systems, using tonometry and smart data tools, make blood pressure checks more correct and easy to use. These systems help people take care of their health with confidence.
Continuous Blood Pressure Monitoring
Pulse Wave Analysis
Pulse wave analysis helps doctors see how blood moves in arteries. This method looks at the shape and timing of each pulse wave. The pulse wave starts at the heart and moves through blood vessels. If arteries get stiff, the wave moves faster. Doctors use this speed, called pulse wave velocity, to guess blood pressure.
- Pulse wave velocity and pulse transit time show how fast the pulse moves. These numbers change when arteries are stiff or relaxed.
- Dual sensors, like photoplethysmography (PPG), can check pulse waves at different wrist spots. This helps get more correct results.
- The pulse wave shape gives clues about the heart’s pumping and blood vessel health. Things like systolic and diastolic times, pulse pressure, and wave shape help guess blood pressure.
- Differences between signals on the back and palm of the hand show how blood flows and bounces back in vessels.
- Using more than one sensor and smart computer programs, doctors can mix information from pulse waves, skin pressure, and temperature. This makes continuous blood pressure checks more trustworthy.
Pulse wave analysis uses these ideas to help the continuous sphygmomanometer give real-time blood pressure numbers. The continuous sphygmomanometer uses models to turn wave shapes into blood pressure numbers. This way works without needles or cuffs, so people can check blood pressure all day.
Pulse wave analysis gives a full view of blood pressure changes. It helps doctors and patients find problems early.
Beat-by-Beat Measurement
Beat-by-beat blood pressure checks show every small change in blood pressure. This method finds quick changes that regular checks miss. For example, people with sleep problems like sleep apnea can have sudden blood pressure jumps at night. These jumps can hurt the heart and blood vessels.
Doctors found that beat-by-beat blood pressure checks can spot early signs of heart and blood vessel problems. In people who had a stroke or mini-stroke, bigger beat-to-beat blood pressure changes meant a higher risk of another stroke. This method gives better warnings than checking blood pressure a few times a day.
Beat-by-beat blood pressure checks also show how the body’s nerves and blood vessels work together. If blood pressure changes too much from beat to beat, it can mean the body is not controlling blood pressure well. This can happen before any symptoms show up. Doctors can use this information to help patients sooner.
SOUSHINE’s continuous sphygmomanometer uses tonometry to check blood pressure for every heartbeat. The sensor has 46 small parts that press gently on the wrist over the artery. This design helps the device catch quick blood pressure changes, even during sleep. The sensor’s special design and smart chip make it strong against noise and keep the readings correct. The continuous sphygmomanometer can show blood pressure changes in real time, helping doctors and patients act fast.
Clinical Impact
Continuous blood pressure checks change how doctors care for patients. When doctors see blood pressure data all day and night, they can make better choices. They can spot problems early and change treatment fast.
- A study showed that patients who got regular nurse follow-ups and teaching had better blood pressure control and felt better. Continuous checks helped nurses and patients work together.
- Remote patient monitoring programs use continuous blood pressure data to help people at home. These programs can lower blood pressure in some groups.
- Doctors can set alerts for when blood pressure goes too high or too low. This helps them act before problems get worse.
The continuous sphygmomanometer gives doctors and patients a clear view of blood pressure patterns. This helps with early finding of high blood pressure, stroke risk, and heart problems. The device’s accuracy and real-time data support better health choices and can improve life quality.
Continuous blood pressure checks with a continuous sphygmomanometer help people stay healthy and avoid serious heart and brain problems.
Blood Pressure Monitors: Wearables

Smart Devices
Wearable technology has changed how people check blood pressure. Now, many people use smartwatches and fitness bands. These devices help people watch their health every day. Wrist-worn blood pressure monitors are very popular. They have advanced sensors and connect to health apps. This makes tracking blood pressure easy.
The table below lists some common wearable blood pressure monitors:
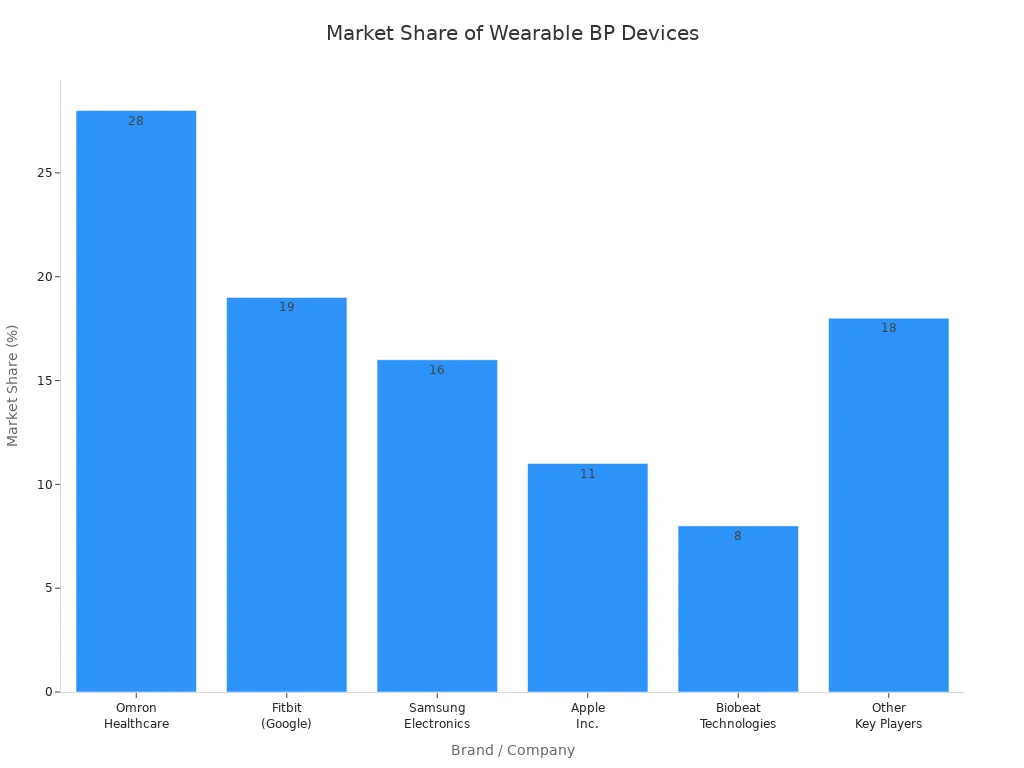
| Company / Brand | Device Type | Technology / Features | Market Share Estimate (%) | Notes |
|---|---|---|---|---|
| Omron Healthcare | HeartGuide™ smartwatch | FDA-cleared, oscillometric technology | 26-30 | First FDA-cleared smartwatch BP monitor, supports remote hypertension management |
| Fitbit (Google) | Sense 2, Charge 6 | PPG-based algorithms for BP trend monitoring | 17-21 | Integrates with health platforms, research mode availability |
| Samsung Electronics | Galaxy Watch series (e.g., Watch6) | Cuffless optical sensors (PPG), requires calibration | 14-18 | Regulatory approvals in Korea, Europe; integrates with Samsung Health apps |
| Apple Inc. | Apple Watch (future models) | Multi-sensor fusion, non-invasive BP trend analysis | 9-13 | Under development, expected advanced digital cardiology integration |
| Biobeat Technologies | Chest patches, wrist devices | FDA-cleared, clinical-grade continuous monitoring | 6-10 | Used in hospitals and homecare for high-risk patient management |
| Other Key Players | Various wrist, upper arm, finger | Cuffless, hybrid cuff, multi-sensor, cloud analytics | 15-20 (combined) | Includes Withings, YHE Technology, Aktiia SA, iHealth Labs, Rivast, Movano, Valencell |
People use these devices at home, work, or while exercising. Many also track heart rate, sleep, and activity.
SOUSHINE Applications
SOUSHINE made a new wrist-wearable device with a multi-element pressure sensor. This device checks blood pressure for every heartbeat. The sensor has 46 small parts and a smart chip. The design keeps the readings correct, even if the user moves or it gets hot or cold.
Engineers tested the SOUSHINE device on a special wrist model. This model acts like real human tissue. The device gave steady and even readings. It was as accurate as regular blood pressure monitors. People can wear the device all day and night. It works during sleep and daily activities. This helps doctors and users see blood pressure changes that old devices might miss.
SOUSHINE’s wearable device helps people manage their health better. It gives real-time data and finds health problems early. The device is easy to wear and does not need a cuff.
Mobile Integration
Mobile health apps are now important for blood pressure checks. These apps connect to wearable devices with Bluetooth. They collect and show blood pressure data right away. Users and doctors see color-coded charts and dashboards. This helps them spot changes and trends easily.
Many systems, like RemoteHealthConnect, use wearables to send data to mobile apps. The apps turn sensor signals into simple charts. Doctors can check patient data from anywhere. They can act quickly if there is a problem. Some apps use machine learning to find risks early.
- Wearable devices collect blood pressure and other vital signs.
- Data goes to mobile apps using Bluetooth.
- Apps show real-time dashboards and trend charts.
- Doctors can watch patients from far away and give care when needed.
- Secure systems keep patient data safe and help with long-term health tracking.
Mobile integration makes blood pressure monitors more helpful. It lets users and doctors work together for better health.
Accuracy and Validation
Clinical Studies
Researchers checked how well wearable blood pressure monitors work in real life. In one study, they compared a wrist device without a cuff to a standard monitor. The wearable gave blood pressure numbers close to the standard device. People said the device was easy to wear every day. But the study did not meet all the rules for accuracy. So, the device cannot take the place of the best monitors yet. The study had people with normal blood pressure. More tests are needed for people with hypertension. Another study in Nature looked at a wristwatch blood pressure monitor. This device was very accurate. Over 85% of its readings were within 10 mmHg of hand-checked numbers. It found hypertension correctly 97.1% of the time. The study said the device needed to be set up for each person. It also needed more tests in different positions. These studies show wearable devices can measure blood pressure well for daily use. But more checks are still needed to make sure they stay accurate.
Regulatory Pathways
Wearable blood pressure monitors must follow strict rules before being sold. Each country has its own rules. The table below lists the main rules:
| Market | Regulatory Authority | Device Classification | Approval Pathways | Conformity Assessment | Quality & Software Standards | Data Privacy Regulations |
|---|---|---|---|---|---|---|
| US | FDA | Class I, II, III | Registration, 510(k), PMA | Premarket notification or approval | ISO IEC 62304:2006 | HIPAA |
| EU | Notified Body under MDR | Risk-based under MDR | CE marking after assessment | Notified Body assessment | ISO IEC 62304:2006 | GDPR |
| China | N/A | N/A | N/A | N/A | N/A | N/A |
The FDA in the US uses a risk system. Class I devices are low risk and need simple steps. Class II devices need 510(k) clearance to show they are safe and work well. Class III devices need more proof and data. The EU uses the MDR system. It also checks risk and needs CE marking. Both places want strong quality and software standards. Privacy rules like HIPAA and GDPR keep patient data safe. Companies must plan early to follow these rules and make sure their devices are correct.
Data Security
Continuous blood pressure monitors send private health data. Keeping this data safe is very important. Developers use many ways to protect it:
- Secure codes and locked channels keep data safe from hackers.
- Devices must follow rules and laws.
- Only allowed people can see health data.
- Updates fix problems and keep devices safe.
- Companies must follow privacy laws to earn trust.
Good data security helps patients feel safe using wearable health devices. Strong protection makes health checks more reliable.
User Benefits
Hypertension Management
Continuous blood pressure monitoring helps people handle hypertension better. Wearable devices check blood pressure all the time, not just sometimes. This way, they catch sudden changes from stress, exercise, or weather. Old methods often miss these quick changes. Now, doctors can see patterns and learn what causes hypertension. They can change treatment fast and give better tips.
Remote monitoring lets doctors watch blood pressure right away. They can help patients and change medicine if needed. This system gives care that fits each person and helps people follow their plans. The table below shows how continuous monitoring is different from old ways:
| Aspect | Continuous Monitoring | Traditional Monitoring |
|---|---|---|
| Frequency | Beat-by-beat, all day | Few times a day or week |
| Data | Shows changes and peaks | Misses many changes |
| Comfort | Wearable, no cuffs | Cuffs can be uncomfortable |
| Use in healthcare | Real-time, remote help | Less data for decisions |
Continuous monitoring gives doctors more facts. They can find risks early and help people control hypertension better.
Early Detection
Finding heart problems early can save lives. Wearable sensors and smart devices now watch blood pressure and heart signals all day. These tools use AI and machine learning to spot trouble before you feel sick. Doctors can see small changes in blood pressure or heartbeats. They can act before things get worse.
- Wearable devices help find hidden hypertension and other heart risks.
- AI models look at health data over time and find patterns.
- Mobile health apps send alerts to doctors when something changes.
- Noninvasive sensors work without stopping daily life.
- Bluetooth and phone apps make sharing health data easy.
These new tools help doctors find problems early. Patients get help faster and avoid big health issues.
Patient Engagement
Wearable blood pressure monitors help people care for their own health. Real-time feedback helps people make good choices and act fast. Many devices link to phone apps. These apps show simple charts and reminders. People check their blood pressure more and learn what changes it.
- Users get reminders to take medicine or check blood pressure.
- Apps use games and rewards to keep people interested.
- People see how food, exercise, and stress change their blood pressure.
- Healthcare teams can send messages and advice right to the user’s phone.
A big study showed people use wearable monitors most in the morning and evening. This regular use helps them build healthy habits. When people see their own health data, they feel more in control. They work with doctors to manage hypertension and keep their hearts healthy.
Wearable monitors make health tracking easy and help people stay close to their healthcare team.
Future Trends
Next-Gen Materials
New materials are making wearable blood pressure sensors work better. Scientists use special materials so sensors can work in many places. Some new ideas include:
- Ti3C2Tx-MXene/PET textile-based sensors bend easily and work well for pulse checks.
- Some flexible sensors use superhydrophobic materials with Joule heating. These sensors do not get wet, even in very humid air.
- Engineers use metals and sodium alginate, which comes from algae, to make sensors last longer and keep water away. Designs like lotus leaves help sensors work when people sweat or go outside.
- Two-dimensional nanomaterials, such as MXene, make sensors more sensitive and bendy.
- New hydrogels let sensors stretch and feel soft on the skin.
- Biodegradable and self-healing materials help sensors last longer and break down safely after use.
- Polymers, liquid metals, and composites are used in many wearable medical sensors. Some use protein-based composites and MXene/protein biocomposites to help the environment.
- Self-healing bases act like human skin and help sensors last longer.
- Advanced printing methods, like inkjet and roll-to-roll gravure printing, make flexible sensors fast and cheap.
These new materials help wearable blood pressure monitors work better every day and support future healthcare.
AI Integration
Artificial intelligence is changing how people check blood pressure. AI models use data from wearable sensors to give more correct readings. Machine learning and deep learning help sort signals like photoplethysmography (PPG). These models clean the data and find important parts. They help guess systolic and diastolic blood pressure more exactly.
AI also helps make blood pressure checks fit each person. The system learns about a person’s habits and changes readings based on sleep or activity. Some AI systems can guess if someone will follow their treatment plan. They can suggest changes to help people manage hypertension. AI-powered apps give feedback and reminders, which can lower blood pressure and help health.
A recent study showed AI can work with fiber optic sensors to check blood pressure during sleep. The system checks how a person sleeps and uses deep learning to keep readings correct. This helps doctors and patients watch blood pressure at night, which is important for managing hypertension. AI makes continuous checks easier and more helpful for healthcare.
Accessibility
Wearable blood pressure monitors are getting more popular. The market for these devices is growing quickly. Many people want easy ways to check their health at home or anywhere. The table below shows how the market is changing:
| Metric | Value | Timeframe | Notes |
|---|---|---|---|
| US market size | $1.2 billion | 2024 | Base year estimate |
| US market size | $3.5 billion | 2033 | Projected market size |
| CAGR (US market) | 12.5% | 2026-2033 | Compound annual growth rate |
| Global market size | $1.53 billion | 2024 | Base year estimate |
| Global market size | $3.19 billion | 2029 | Projected market size |
| CAGR (global) | 16.2% | 2024-2029 | Compound annual growth rate |
| Key growth factors | Regulatory approvals, technological innovation, consumer preferences, healthcare accessibility | – | Factors influencing adoption |
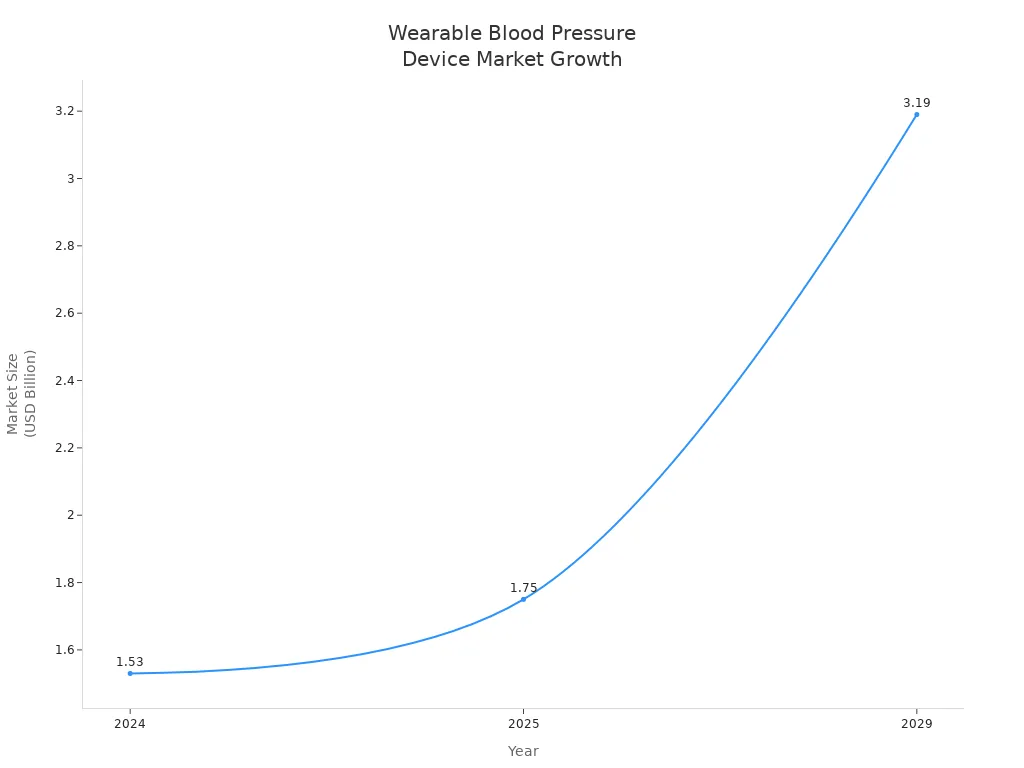
Doctors and patients both get help from these new devices. More people can check blood pressure without going to a clinic. As technology gets better, wearable monitors will be even easier to use. This growth helps make healthcare easier for everyone.
New sensor breakthroughs have made blood pressure monitors better. SOUSHINE’s multi-element sensor gives readings that are correct and easy to trust. Wearable devices now help people check their health every day. In the future, wearable health technology might have:
- Devices that disappear after being used
- Flexible sensors made with special new materials
- E-tattoos that watch the skin
- Smart contact lenses that check eye health
- Sensors that track air quality and medicine
These new ideas will help more people take care of their health and find problems sooner.
FAQ
What makes SOUSHINE’s multi-element pressure sensor different?
SOUSHINE’s sensor has 46 sensing elements and a special chip. This setup gives accurate blood pressure readings for every heartbeat. The sensor works well even if you move or the temperature changes.
Can people wear the device all day and night?
Yes. The device is made from soft, skin-friendly materials. You can wear it while you sleep, work, or exercise. The sensor keeps working and does not feel uncomfortable.
How does the device send blood pressure data to doctors?
The device links to health apps on your phone using Bluetooth. The app shows charts and trends right away. Doctors can see your data from far away and give advice.
Is the sensor safe for skin contact?
Yes. SOUSHINE uses safe resin and other safe materials. The sensor does not bother your skin. The design keeps both you and the sensor safe.
How accurate is the SOUSHINE wearable compared to traditional monitors?
Studies show SOUSHINE’s device is as accurate as cuff monitors. The sensor gives steady readings for daily use and medical care.
Who can benefit from continuous blood pressure monitoring?
People with hypertension, heart disease, or sleep problems can benefit. Athletes and people who want to watch their health trends also find it helpful.
Tip: Always listen to your doctor when using any health device.